TNM classification 9ᵗʰ edition
Onno Mets and Robin Smithuis
Radiology department of the University Medical Center Amsterdam and the Alrijne Hospital, Leiden, the Netherlands
Publicationdate
This document summarizes the 9th Edition of the TNM Classification for Lung Cancer, which became the standard for lung cancer staging as of January 1, 2025. The classification is issued by the International Association for the Study of Lung Cancer (IASLC) and supersedes the 8th Edition.
Introduction
Purpose of TNM Classification
The TNM classification provides a standardized nomenclature for describing the anatomic extent of disease, facilitating consistent communication regarding patient outcomes and the applicability of clinical data to individual cases.
Scope of Application
The TNM classification system for lung cancer applies to both non-small cell lung carcinoma (NSCLC) and all neuroendocrine neoplasms, including small cell lung carcinoma (SCLC) and typical carcinoid tumors. It does not apply to pulmonary sarcomas, lymphomas, or other rare tumors.
Tables of the TNM 9ᵗʰ edition
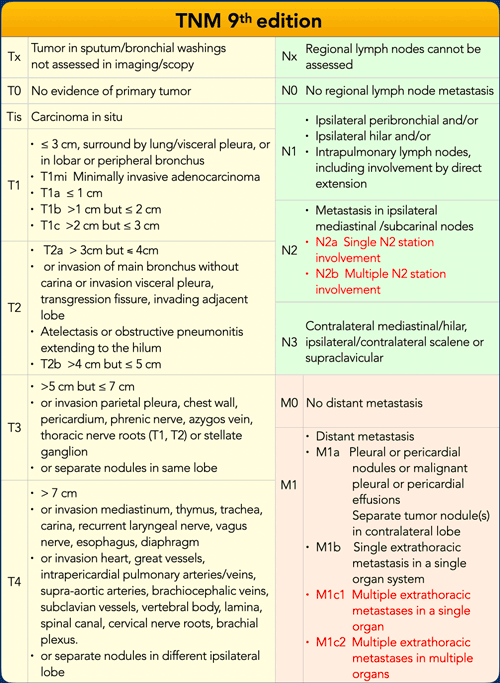
TNM 9ᵗʰ edition
Key Updates in the 9th Edition
The 9th Edition of the lung cancer TNM classification is presented in the accompanying table. Notable changes from the 8th Edition are highlighted in red:
- T Component: No changes.
- N Component: N2 involvement is now subdivided into N2a (single N2 station) and N2b (multilevel stations).
- M Component: M1c status is further subdivided into M1c1 (multiple metastases in a single organ system) and M1c2 (metastases in multiple organ systems).
These revisions result in a rearrangement of certain stage groups, as detailed in the subsequent table.
Prefixes and Evaluation Categories
Several prefixes specify the context of TNM classification:
- Clinical Stage (c): Determined using all available pretreatment information.
- Pathologic Stage (p): Defined by findings following surgical resection; use is restricted to this context.
- Restaging (y): Applied after partial or complete treatment, either in the absence of resection (ycTNM) or following resection (ypTNM).
An evaluation categorization (‘E’) is recommended to indicate the type of diagnostic testing:
- E1: Physical examination
- E2: Imaging
- E3: Tissue sampling (E3a: cytology; E3b: histology)
- E4: Resection
Examples:
- cT2aN2aM0 E3a: Cytologic confirmation of N status used for pretreatment staging.
- pT1cN0M0 E4: Staging based on definitive resection.
Subsolid lesions
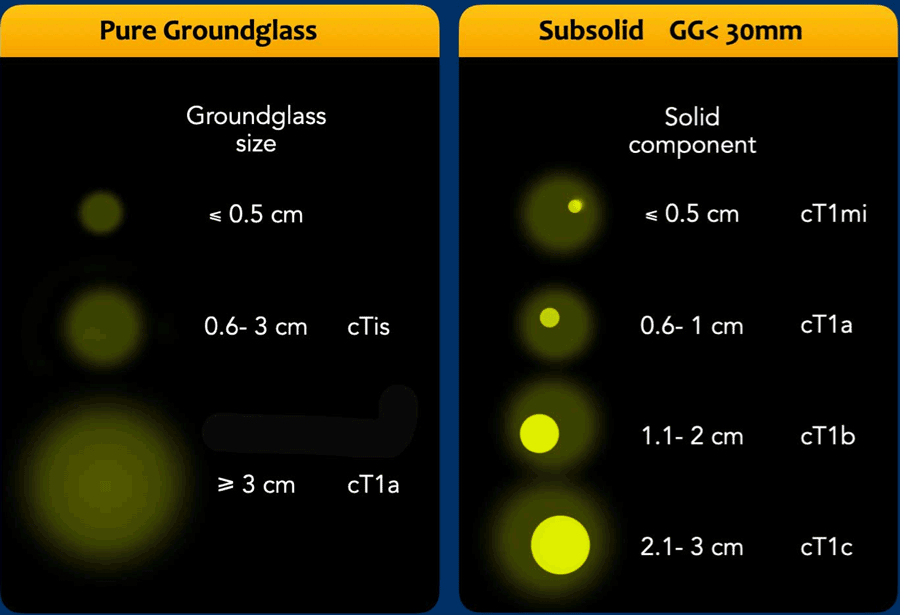
Subsolid lesions in lung cancer exhibit ground-glass morphology, reflecting lepidic growth—defined as tumor cells proliferating along alveolar surfaces without invasive growth. These lesions may or may not contain an internal solid component, which is presumed to represent the invasive portion of the tumor.
Radiologic Assessment Radiology reports for subsolid lung cancers must document both the total lesion size and, if present, the dimensions of any solid component. Measurements should be obtained from contiguous thin-slice (<1.5 mm) CT reconstructions in lung window settings.
Classification of Subsolid Lung Cancers
Subsolid lung cancers are classified as illustrated in the accompanying figures.
- Pure Ground-Glass Lesions
- Lesions ≤30 mm in total size are classified according to the greatest total dimension and may be designated as carcinoma in situ (cTis) at most.
- Lesions >30 mm are classified as at least cT1a, irrespective of pure ground-glass or part-solid morphology.
- Part-Solid Lesions (Ground-Glass with Solid Component)
- When a solid component is present, classification is based on the greatest dimension of the solid component, which is presumed to represent the invasive component on histopathology.
- For example:
- A total lesion size ≤30 mm with a solid component ≤5 mm is classified as cT1mi (minimally invasive).
- A total lesion size >30 mm with a solid component ≤5 mm is classified as cT1a, as the total lesion size exceeds the 30 mm threshold for cT1a classification.
- Depending on the size of the invasive component, part-solid lesions may also be classified as cT1b (solid component 11–20 mm) or cT1c (solid component 21–30 mm).
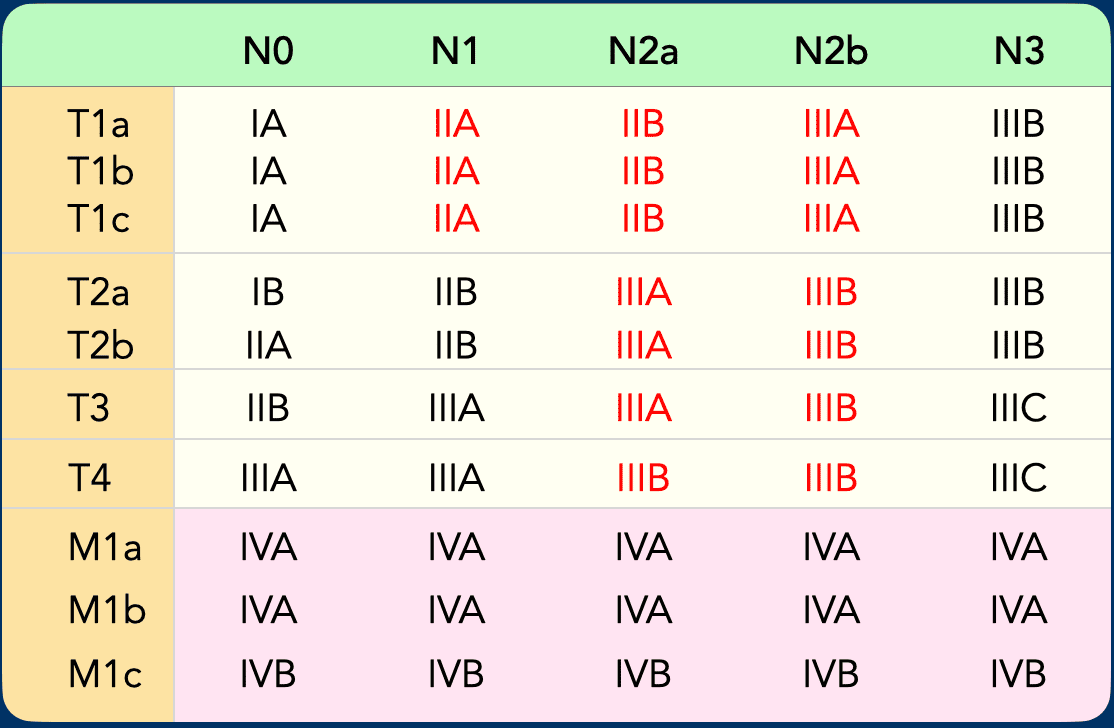
TNM Staging and Prognostic Grouping
Subsets of T, N, and M categories are consolidated into distinct stage groups, as patients within each group exhibit similar prognostic outcomes.
For example, cT1N0M0 disease (stage IA) is associated with a 5-year survival rate of approximately 82%.
Conversely, M1c disease (stage IVB) demonstrates a 5-year survival rate of about 7%.
The 9th Edition of the TNM classification introduces a rearrangement of T and N categories within stage groups IIA, IIB, IIIA, and IIIB (see Table).
All other stage categories remain unchanged from the previous edition.
T-staging
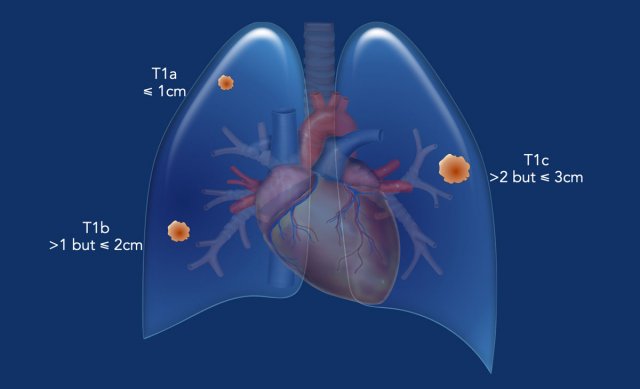
T1 - T4
T1 Tumor
Tumor size is determined by the greatest dimension of the invasive component, based on either pathological examination or clinical data (i.e., the solid component on contiguous thin-slice CT reconstructions in lung window settings).
The largest tumor dimension may be identified on multiplanar reconstructions rather than the axial plane alone.
T1-tumor (≤ 3 cm, surrounded by lung/visceral pleura, or in lobar or more peripheral bronchus).
- T1mi: Minimally invasive adenocarcinoma.
- T1a: Tumor ≤1 cm in greatest dimension.
- T1b: Tumor >1 cm but ≤2 cm in greatest dimension.
- T1c: Tumor >2 cm but ≤3 cm in greatest dimension.
Example:
A typical T1 tumor in the left lower lobe (23 mm, cT1c), completely surrounded by pulmonary parenchyma.
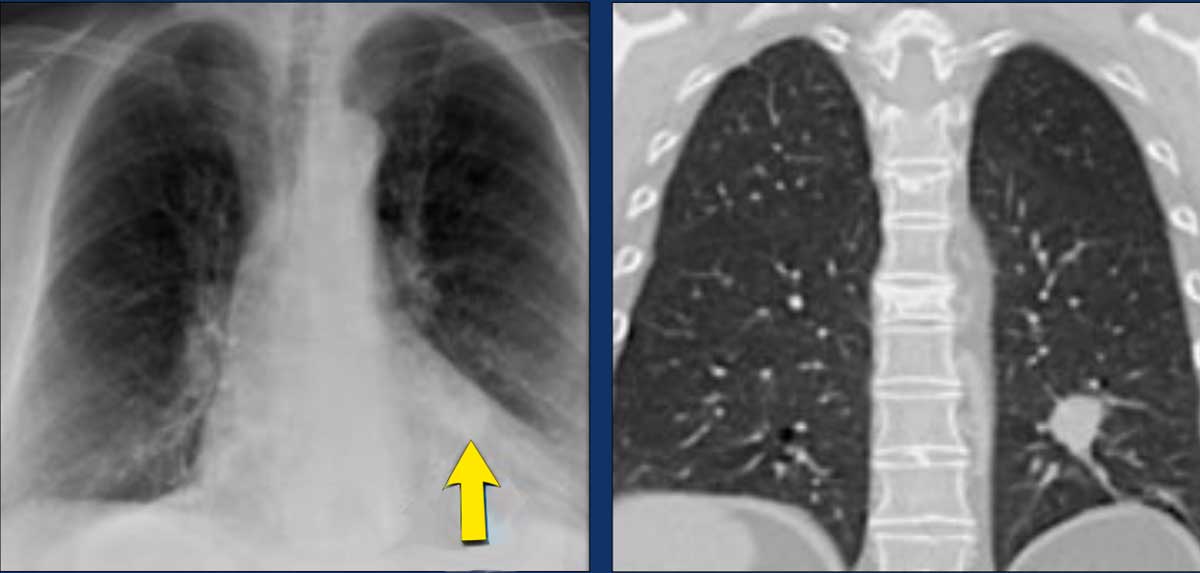
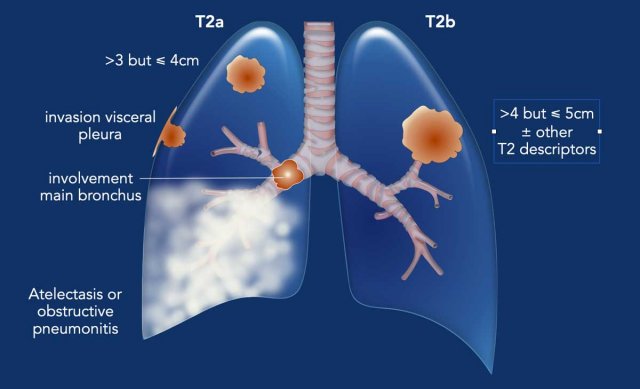
T2 Tumor
A T2 tumor is characterized by any of the following features:
- T2a:
- Tumor >3 cm but ≤4 cm in greatest dimension.
- Invasion of the visceral pleura or adjacent lobe.
- Involvement of the main bronchus (not including the carina).
- Association with atelectasis or obstructive pneumonitis extending to the hilar region, involving part or all of the lung.
- T2b:
- Tumor >4 cm but ≤5 cm in greatest dimension, with or without other T2a features.
Example:
A typical T2 tumor with atelectasis/pneumonitis of the left lower lobe extending to the hilum, secondary to left lower lobe bronchus involvement (31 mm, pT2a).
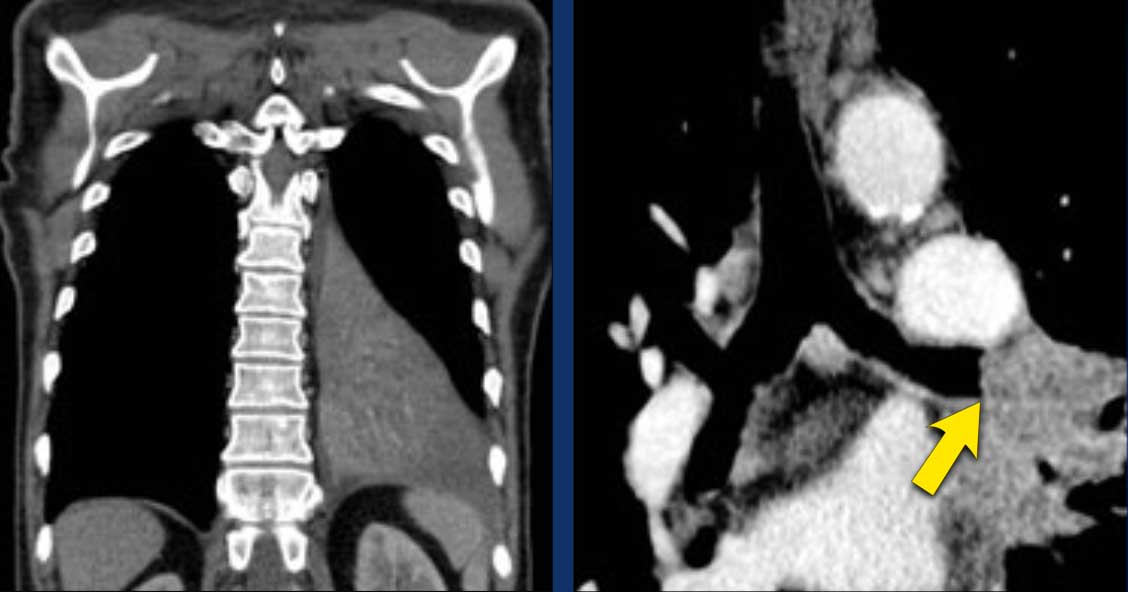
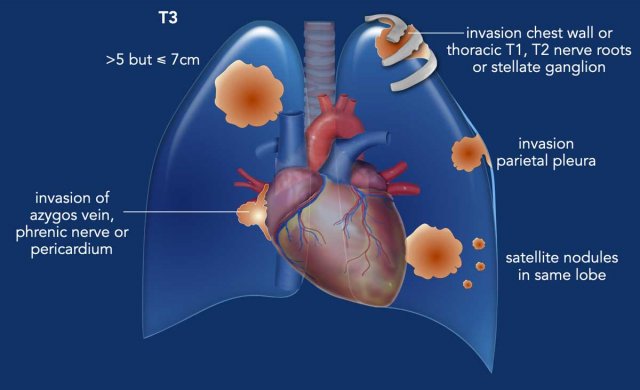
T3 Tumor
A T3 tumor is defined by any of the following features:
- Tumor >5 cm but ≤7 cm in greatest dimension.
- Invasion of the parietal pleura or chest wall.
- Invasion of the pericardium, phrenic nerve, or azygos vein.
- Invasion of thoracic nerve roots (e.g., T1, T2) or stellate ganglion.
- Presence of separate tumor nodule(s) in the same lobe as the primary tumor.
Notes:
- Direct invasion of adjacent structures (e.g., phrenic nerve, aorta, chest wall) by the primary tumor is considered for T category determination.
- Direct invasion into lymph nodes is classified as lymph node involvement (N category).
- Direct invasion of an extrathoracic organ (e.g., liver) is not classified as M1 involvement.
Example:
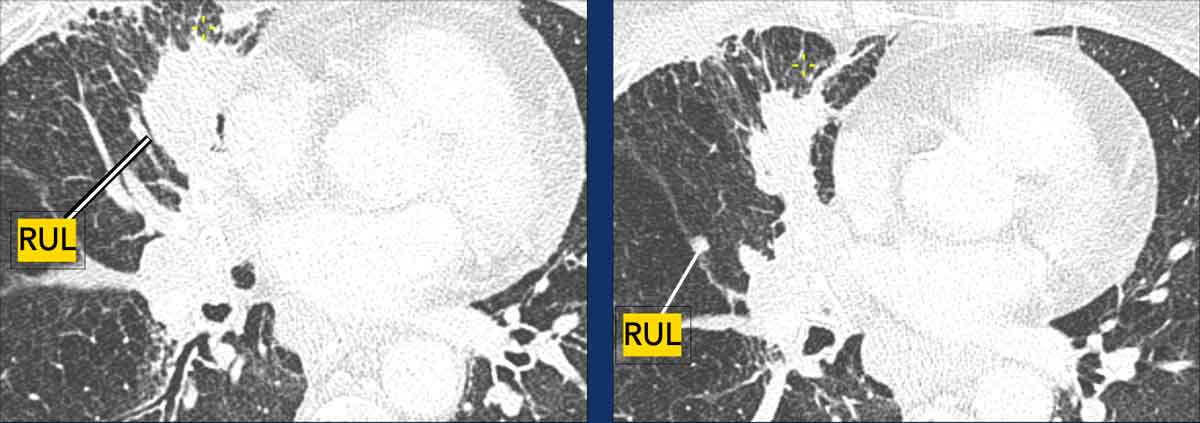
A
typical T3 tumor in the right upper lobe with invasion of the chest wall (59
mm, cT3).
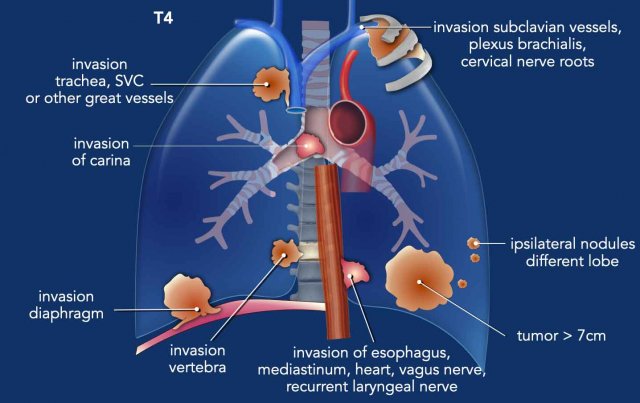
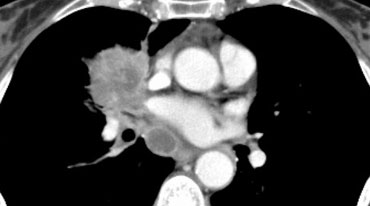
T4 Tumor
A T4 tumor is defined by any of the following features:
- Tumor >7 cm in greatest dimension.
- Invasion of the mediastinum, thymus, trachea, carina, recurrent laryngeal nerve, vagus nerve, esophagus, or diaphragm.
- Invasion of the heart, great vessels, intrapericardial pulmonary arteries/veins, supra-aortic arteries, brachiocephalic veins, subclavian vessels, vertebral body, lamina, spinal canal, cervical nerve roots, or brachial plexus.
- Presence of separate tumor nodule(s) in a different ipsilateral lobe.
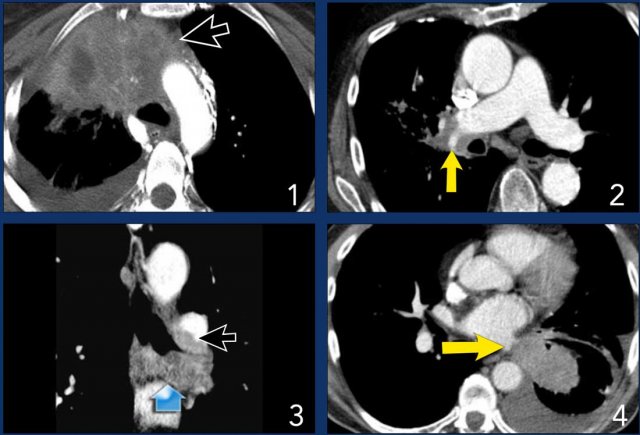
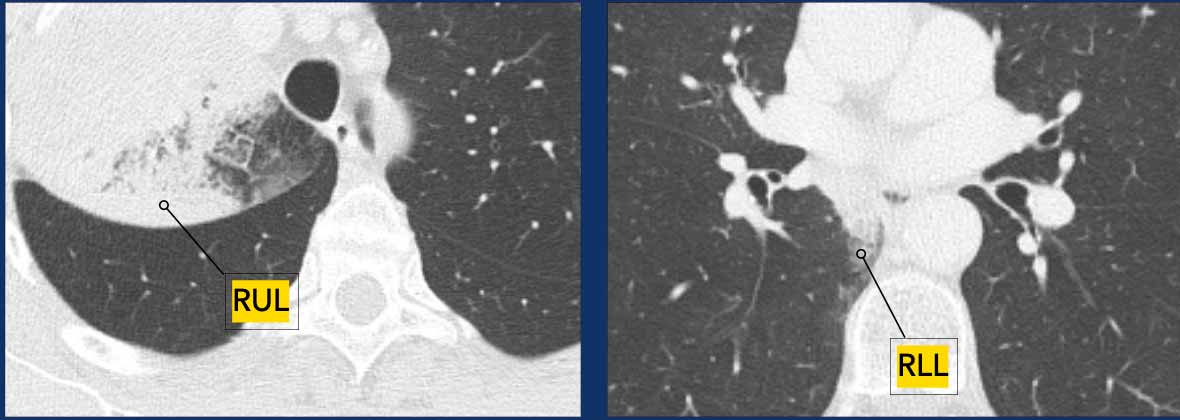
Example:
- A typical T4 tumor in the right upper lobe with invasion of the mediastinum.
- Invasion of the right pulmonary artery.
- Invasion of the carina.
- Invasion of the left atrium.
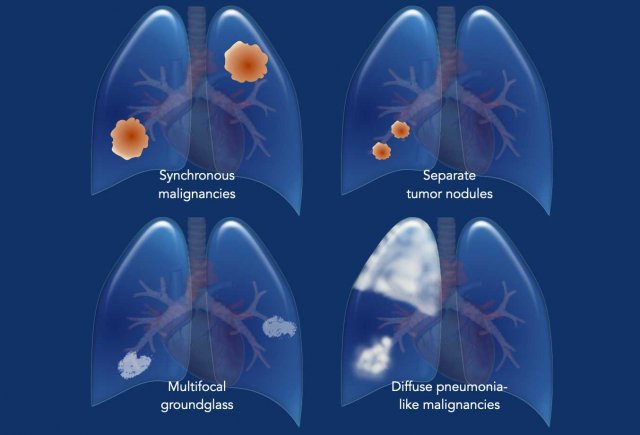
Staging multiple sites of malignancy
In some cases, multiple sites of lung cancer are suspected in a single patient.
It is essential to determine the nature of multifocality, as different patterns exhibit distinct biological behaviors and are subject to specific TNM classification rules.
The following patterns are recognized:
- Synchronous Primary Malignancies
- Separate tumor nodules of the same malignancy
- Multifocal Ground-Glass or Lepidic Lesions
- Diffuse Pneumonia-Like Malignancies
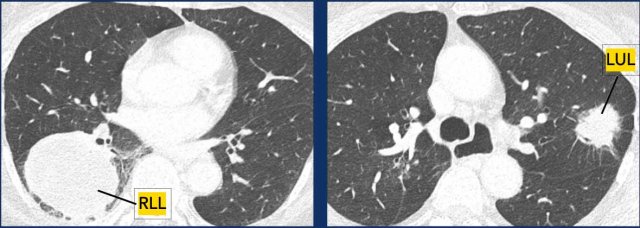
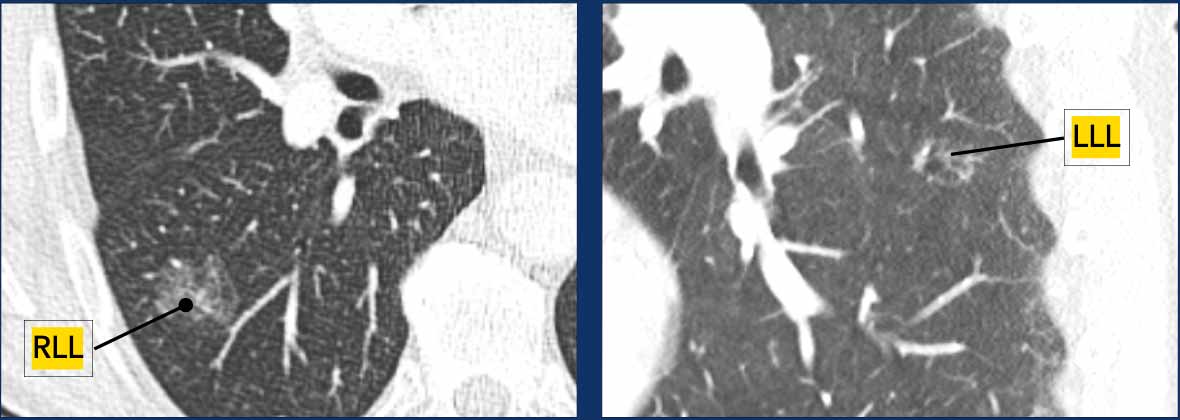
1.Synchronous Primary Malignancies
- Each tumor is staged separately with its own TNM classification. Example:
Examples
- T4N0M0 in the right lower lobe (RLL).
- T2bN1M0 in the left upper lobe (LUL).
2. Separate Tumor Nodules of the Same Malignancy
- T3: If nodules are located in the same lobe.
- T4: If nodules are in the same side but different lobes.
- M1a: If nodules are in the contralateral lobe.
- A single N and M category is assigned for all nodules.
Example:
- T3N2aM0 in the right upper lobe (RUL), with T3 classification based on a separate nodule in the same lobe.
3. Multifocal groundglass or lepidic lesions
- The T-stage is determined by the most dominant lesion.
- A single N and M category is assigned for all lesions.
- Multiplicity is indicated as (#/m), for example, three lesions are denoted as 3/m.
Example:
- T1aN0M0 (2/m), with T1a classification based on the dominant lesion in the RLL.
4. Diffuse pneumonia-like malignancies
- T3: If confined to the same lobe.
- T4: If present in the same side but different lobes.
- M1a: If present in the contralateral lobe.
- A single N and M category is assigned for all lesions.
Example:
- T4N1M0, with T4 classification based on the lesion in the RLL.
N-Staging
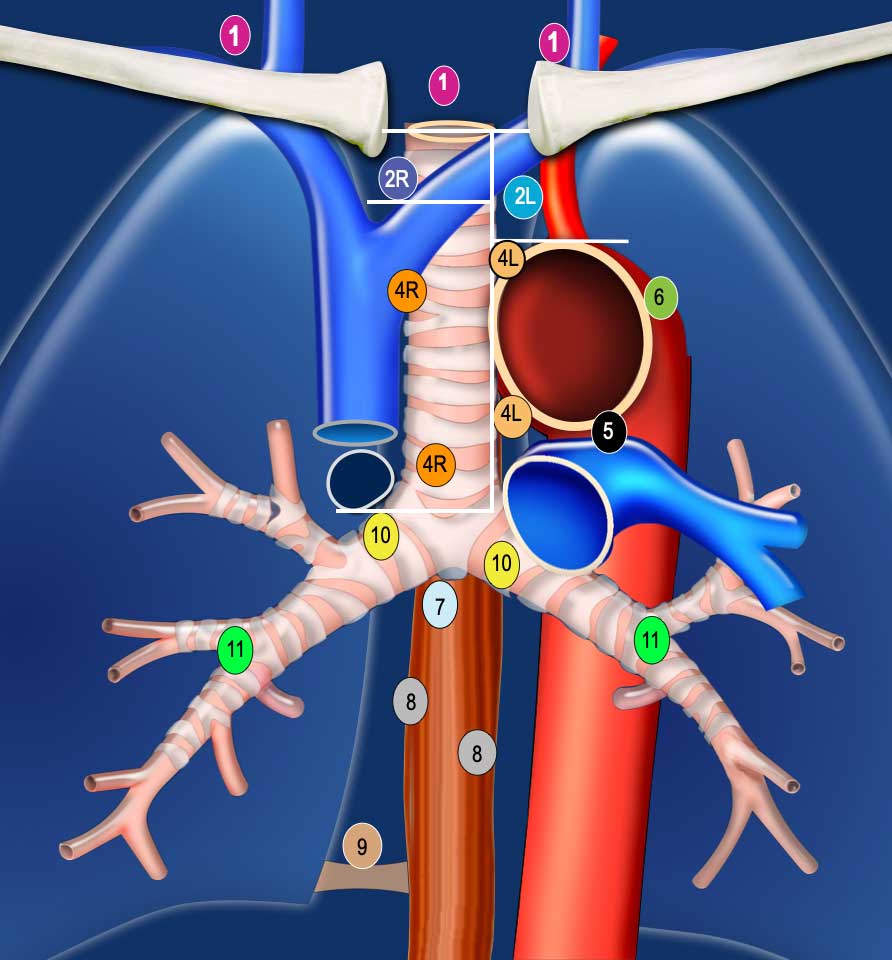
Regional Lymph Node Classification System
Regional lymph node involvement in lung cancer encompasses intrathoracic, scalene, and supraclavicular lymph nodes. Involvement of less common sites, such as parasternal or axillary nodes, is considered metastatic disease.
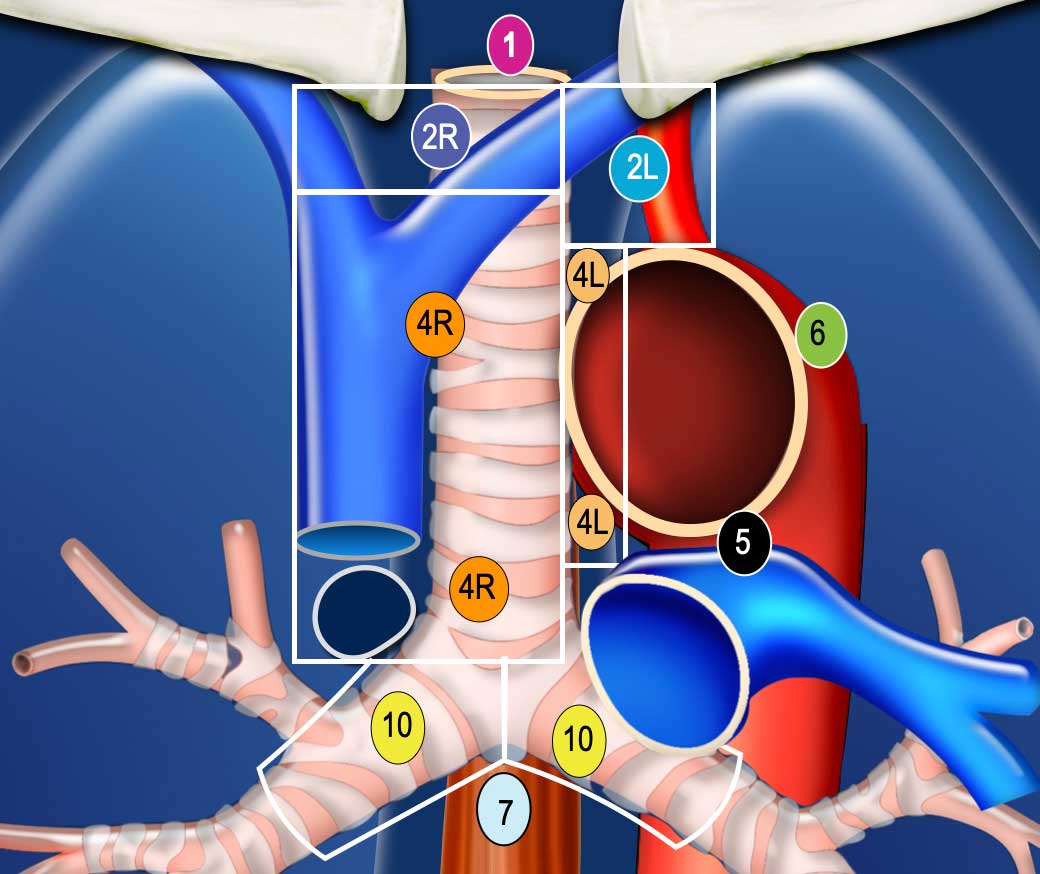
The International Association for the Study of Lung Cancer (IASLC) lymph node map is utilized for classification:
- Low cervical, supraclavicular, and sternal notch nodes
- Upper paratracheal nodes
- Pre-vascular (3A): Nodes anterior to the vessels, not adjacent to the trachea
- Pre-vertebral (3P): Nodes posterior to the esophagus, in the prevertebral space
- Lower paratracheal nodes
- Subaortic (aortopulmonary window) nodes
- Para-aortic (ascending aorta or phrenic) nodes
- Subcarinal nodes
- Paraesophageal nodes
- Pulmonary ligament nodes: Located within the pulmonary ligaments
- Hilar nodes: Located outside the mediastinum
Diagnostic Imaging
CT is unreliable for staging lymph nodes in patients with non-small cell lung cancer (NSCLC), regardless of the size threshold chosen.
PET-CT is significantly more reliable for determining N-status, although false positives may occur in conditions such as sarcoidosis, tuberculosis, and other infections.
PET-CT demonstrates a high negative predictive value.
IASLC Lymph Node Level Definitions
- Level 1 (N3): Includes low cervical, supraclavicular, and sternal notch nodes. The lower border is the clavicles bilaterally and, in the midline, the upper border of the manubrium. There is an important separation to be made between level 1 (N3) and level 2 and 3 nodes (N2).
- Level 2R: The upper border is the lung apex and, in the midline, the upper border of the manubrium. The lower border is the intersection of the caudal margin of the innominate vein with the trachea. The medial border is the left lateral border of the trachea.
- Level 2L: Extends from the lung apex and the upper border of the manubrium to the superior border of the aortic arch.
- Level 4R: Includes right paratracheal and pretracheal nodes, extending to the left lateral border of the trachea, from the intersection of the caudal margin of the innominate vein with the trachea to the lower border of the azygos vein.
- Level 4L: Nodes to the left of the left lateral border of the trachea, but medial to the ligamentum arteriosum, from the upper margin of the aortic arch to the upper rim of the left main pulmonary artery.
- Level 5: Subaortic nodes lateral to the ligamentum arteriosum, not located between the aorta and the pulmonary trunk.
- Level 10R: Hilar nodes up to the inferior border of the azygos vein, including those in a precarinal position.
- Level 10L: Hilar nodes extending up to the upper border of the left pulmonary artery.
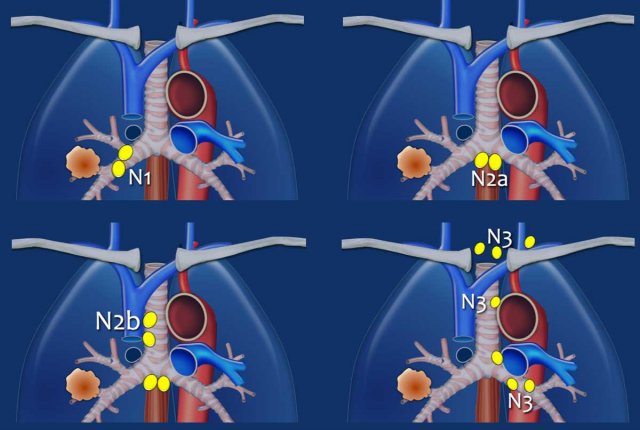
N1 - N3 nodes
Nodal Staging Definitions
- N1: Metastasis in ipsilateral intrapulmonary, peribronchial, or hilar lymph nodes, including direct extension.
- N2a: Metastasis to a single ipsilateral mediastinal or subcarinal lymph node station.
- N2b: Metastasis to multiple ipsilateral mediastinal and/or subcarinal lymph node stations.
- N3: Metastasis in contralateral hilar or mediastinal lymph nodes, or in scalene or supraclavicular lymph nodes.
N1 nodes
N1-nodes are ipsilateral nodes within the lung and hilar nodes.
N1 alters the prognosis but not the management.
Example:
T2a
tumor (33 mm) in the right lower lobe with ipsilateral hilar node metastasis
(N1).
N2 Nodes
N2 nodes represent ipsilateral mediastinal or subcarinal lymphadenopathy.
- N2a: Single N2 station involvement
- N2b: Multiple N2 station involvement
Example: A right-sided tumor with lymph node metastases in multiple ipsilateral mediastinal stations (4R and 2R) is classified as N2b.
N3 Nodes
N3 nodes represent contralateral mediastinal or hilar lymphadenopathy, or scalene or supraclavicular nodes, and are considered irresectable.
Example:
A right-sided tumor with N3 lymph node metastases, including contralateral mediastinal stations 4L and 5.
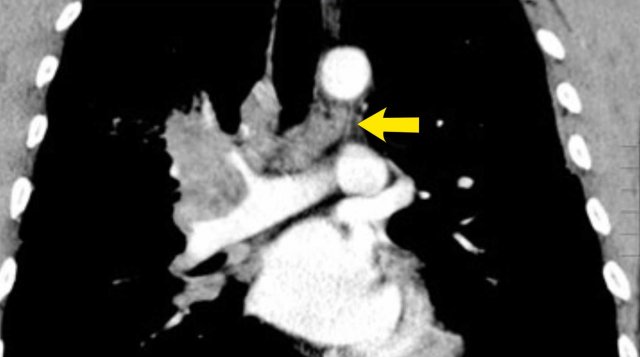
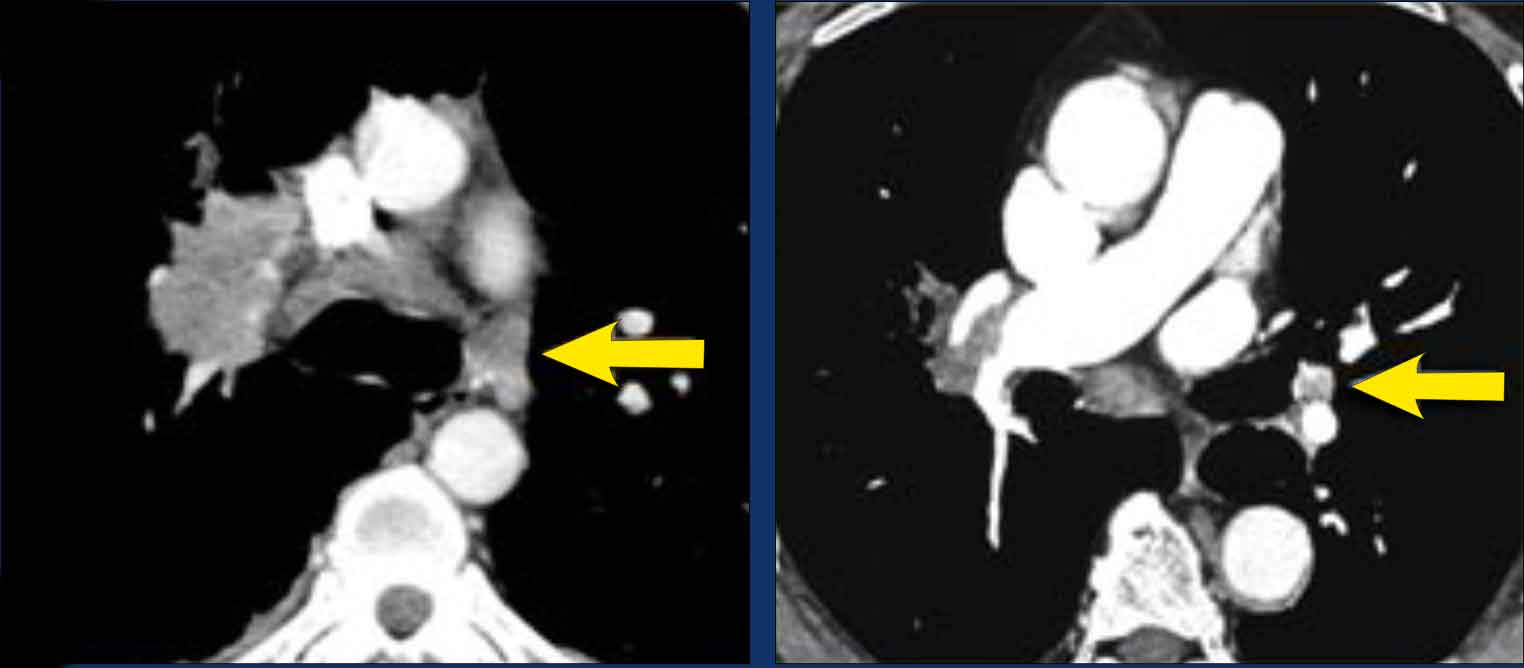
These images are of two different patients with lung cancer in the right lung.
Images
There are lymph nodes on the contralateral side.
If these lymph nodes contain tumor cells, it means N3 disease.
Images of a patient with a right sided tumor.
There are N3-nodes on the contralateral side and in the right supraclavicular region.
Scroll through the images.
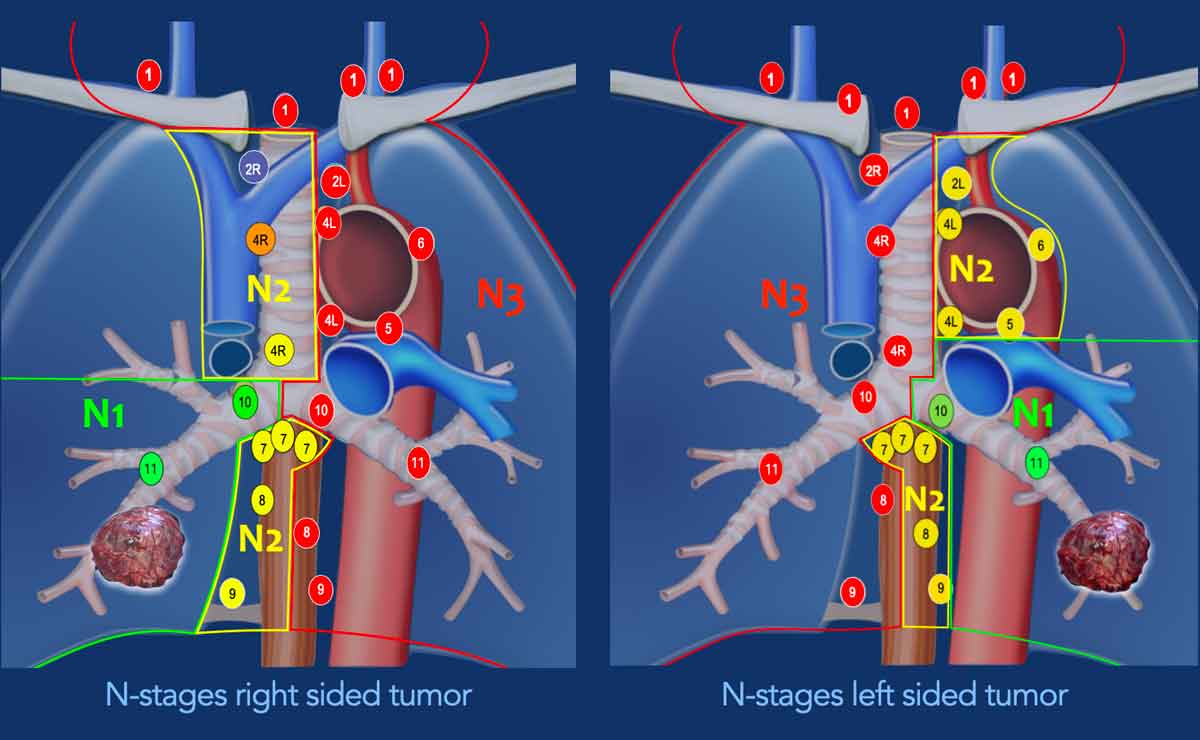
Nodal Staging by Tumor Laterality
Right Lung Tumors:
- N1: Ipsilateral peribronchial and/or hilar lymph nodes (10R–14R)
- N2: Ipsilateral mediastinal and/or midline lymph nodes (2R, 3A/P, 4R, 7, 8R, 9R)
- N3: Contralateral mediastinal and/or hilar, and any supraclavicular lymph nodes (1, 2L, 3AL, 4L, 5, 6, 8L, 9L, 10L–14L)
Left Lung Tumors:
- N1: Ipsilateral peribronchial and/or hilar lymph nodes (10L–14L)
- N2: Ipsilateral mediastinal and/or midline lymph nodes (2L, 3A/P, 4L, 7, 8L, 9L)
- N3: Contralateral mediastinal and/or hilar, and any supraclavicular lymph nodes (1, 2R, 3AR, 3PR, 4R, 8R, 9R, 10R–14R)
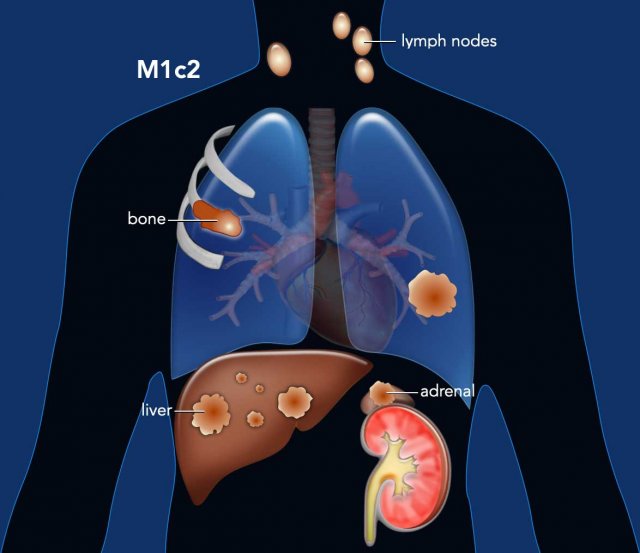
M-Staging
M-staging
is based on the presence of metastases, their location and multiplicity.
M0 is no metastases and M1 means distant metastases.
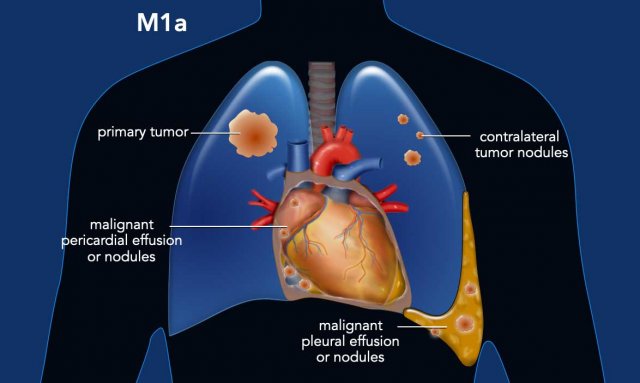
A distinction is made between regional or intrathoracic metastatic disease
(M1a) and distant metastatic disease, either solitary (M1b) or multiple (M1c),
in a single organ system (M1c1) or in multiple organs (M1c2).
Figure
M1a: Regional
(or intrathoracic) metastatic disease defined as malignant pleural or
pericardial effusion or nodules, as well as contralateral separate pulmonary
nodules.
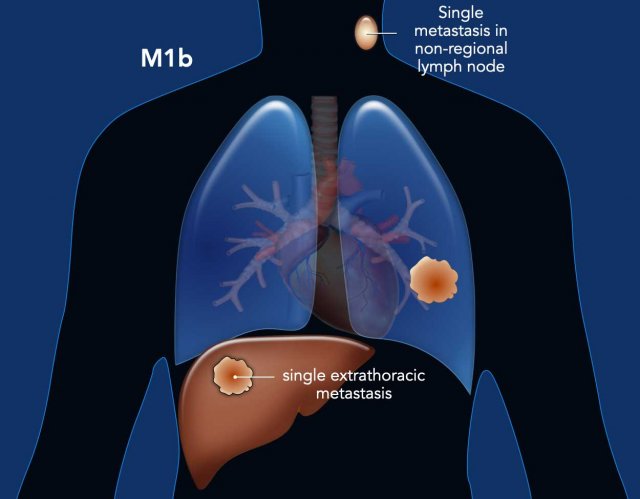
M1b is a single extrathoracic metastasis in a single organ system. It is important to emphasize, that an organ system denotes all sites of an organ system distributed throughout the body, or both sides in case of a paired organ.
This means that multiple lesions in different sites of the skeletal system or
the skin is M1c1 disease.
However,
multiple lesions in both the skeletal system and the adrenals is M1c2 disease.
Figure
M1b: Single extrathoracic metastasis in a single organ system.
This can be in a non-regional lymph node (without a liver metastasis) or a single metastasis in the liver (without a non-regional lymph node).
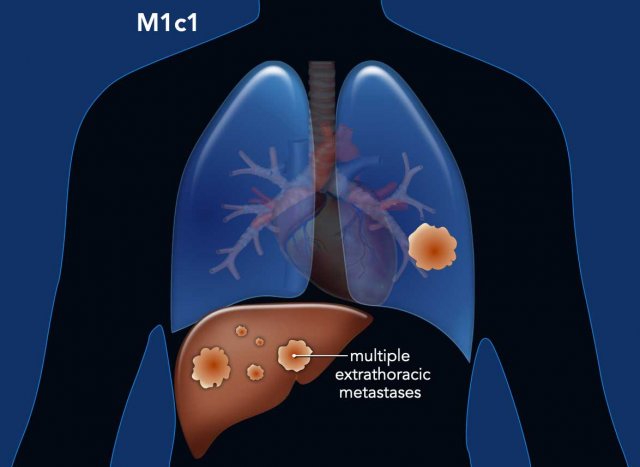
Figure
M1c1: Multiple extrathoracic metastases in a single organ.
Almost every organ may be involved in metastatic disease.
Metastases are commonly seen in the adrenals, lymph nodes, the brain, bones and liver.
Figure
M1c2: Multiple extrathoracic metastases in multiple organs systems.